Transitional Digital Pathology
Success Measurement
Strategic Initiative
Over the past decade, there has been an explosion of technological capabilities which has revolutionized medical research. In the past, scientists studied one “molecule” at a time providing little knowledge on how these molecules interact with one another and hence little insight on the biological pathways or processes that are disrupted in the development of disease.
Today, researchers are able to undertake a more ‘holistic’ view. Recent advances in innovative omics technologies allow for the comprehensive or global profiling of a set of molecules. Genomics was the first omics discipline; unlike ‘genetics’ where studies involve individual variants or single genes, genomics focuses on the entire genome (DNA). With more cost-efficient and high-throughput technologies now available, omics-based research has become routine. Integration of multiple types of omics data, known as multi-omics, lends the opportunity to elucidate disease mechanism and causality, or identification of potential therapeutic targets.

In spite of the wealth of omics data available in studies of cancers, the translation of these research findings have been painstakingly slow. An example is the genome-wide studies of cancers; through this work, we know that cancers of the same cell type, origin, and stage have unique molecular features that could impact course of disease and response to treatment. Although these specific molecular features offer great promise for the development of personalized cancer care, the current management of cancers i.e. diagnosis still largely relies upon a patient’s tumour cell type assessed through examining the pathology tissue slides under the microscope and the stage of the cancer, without further refinement. Even when distinct diagnostic modalities are used to aid in management, they are done as disconnected parallel activities and without the synergy obtainable through leveraging the vast data available.
Recent advances in artificial intelligence (AI) techniques have shown impressive performances in many challenging applications. In pathology, AI techniques have allowed computers to interpret pathology slide images and infer information from the tumor tissue that is not discernable to the human eye. One study has even been able to correlate histopathology imaging features (currently not appreciated by traditional microscopy) with genetic mutation status in lung adenocarcinomas. As such, these recent advances, fueled by the digitization of the traditional histopathology tissue slides, offers the opportunity to objectively revisit the rich amount of information in pathology slides.
This initiative proposes to overcome one of the largest obstacles within the research-to-practice continuum; limited capacity to translate genomic basic science discoveries to the bedside. This obstacle is a direct outcome of shortfalls in clinical resources, translational pathology expertise, facilitating infrastructure, and interdisciplinary informatics expertise. In BC, we have a unique opportunity to close this gap and build a leading edge centre focused on artificial intelligence (AI) applications in pathology and medicine. The GCI will take advantage of BC’s cancer care system (with a single payer system and uniform treatment protocols, together with excellent quality patient outcome data) and leverage the world-class team of clinicians, scientists, and engineers in the province with complementary expertise in pathology, artificial intelligence, genomics, and imaging to accelerate this line of research with the goal of improving the diagnostics and management of women faced with a diagnosis of gynecologic cancer.
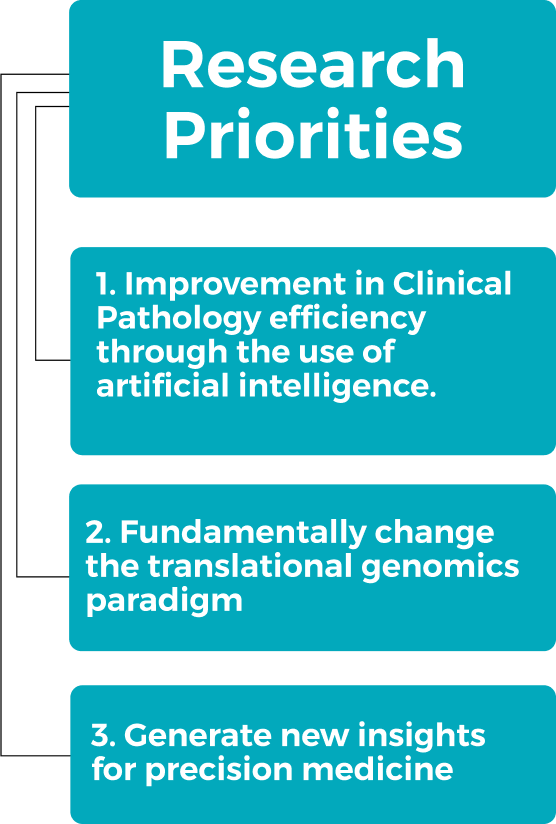
This initiative has three pillars of research:
1. Improvement in Clinical Pathology efficiency through the use of artificial intelligence.
The goal is to improve efficiency by pre-screening pathology histological slides prior to review by a pathologist; this will enable triaging of more complex and difficult cases for expert examination and/or additional molecular testing.
2. Fundamentally change the translational genomics paradigm
Artificial intelligence will be utilized to identify features in histological images that can predict genomic subtypes or features. By removing the need to perform genomic tests which may not be readily available in all pathology labs or hospitals, or is costly, this will enable the rapid and accurate stratification of patients into clinically relevant genomic subgroups.
3. Generate new insights for precision medicine
This pillar aims to identify new biomarkers that can improve upon the risk stratification of patients with the goal of improving the current standard of care. We will embrace the unique multi-modal data available which comprises of a combination of genomics, histopathology, and imaging; through a multi-modal approach, there is a greater opportunity to identify novel markers as each data modality provides additional information which is not possible to obtain from individual data sources.
While the current proposal focuses on two gynecologic cancer sites – the ovary and the endometrium, all advanced artificial intelligence techniques developed can be applied to other sites. The key resources we have previously built in these two areas (described below) are critical to the success of this initiative and enables the research proposed.
I. Ovarian Cancer
Major ovarian cancer histotypes have distinct cellular morphologies and etiologies, as well as molecular, genetic, and clinical attributes. However, standard clinical management of these histotypes is similar and patient outcomes have not seen any improvements. Recent genomic and molecular sub-classifications of ovarian cancer (including ours published in Nature Genetics3) potentially have important clinical implications, including identification of new therapeutic targets. However, until the discovery of surrogate biomarkers these sub-classifications are based on labor-intensive assays using fresh or snap frozen tumour samples, with long turn-around times, limiting their routine use as treatment must start soon after diagnosis.
Histology has been an important tool in cancer diagnosis and prognostication for more than a century. This phenotypic information reflects the aggregate effect of molecular and genetic alterations on cancer cells and provides a convenient visual readout of disease biology. Histology presents a wealth of information that is not easily accessible through genomics techniques, is inexpensive to acquire, and is the cornerstone for cancer diagnosis and management.
We will leverage our ability to access 10,000 ovarian cancer cases (largest in the world) with histopathology images, clinical outcome and genomic data which are derived from >60 contributing groups around the world. Using this rich resource, we propose to build a platform for characterizing ovarian cancer, based on advanced artificial intelligence techniques, and by combining genetic and histology markers. More specifically, we will build automated differential diagnostic tool for major ovarian cancer subtypes, investigate the relationship between genetic markers, histology and disease outcome, and combine these data for a comprehensive profile of each tumour. New knowledge generated from this project will shed light on the link between histology and genetic markers and identify potential biomarkers that can be rapidly and accurately tested to stratify ovarian cancer for accurate treatment selection.

~7,000 Canadian women are diagnosed with Endometrial carcinoma every year.
Traditionally histopathology is used to diagnose endometrial cancer; however endometrial cancers are difficult to tell apart under the microscope. Consequently, clinicians struggle to determine ‘the best’ treatment for patients. As a result, many women may be getting unnecessary toxic treatments when surgery alone can cure them and conversely, many women do not receive the aggressive treatments they need that could be tailored to the unique biology of their cancer.
Recent advances in molecular pathology and precision medicine have led to a re-classification of endometrial carcinomas. Now endometrial carcinomas can be genetically profiled and classified into four prognostically distinct groups: ultramutated, hypermutated, copy number low, and copy number high. Unfortunately, this genetic classification is expensive and labour-intensive with long turn-around times. In BC, we have been the first to develop a pragmatic tool (ProMisE) that can reliably distinguish endometrial cancers by molecular features. This tool will soon be tested in a clinical trial setting to determine its utility and ability to change treatment paradigms. This initiative proposes to leverage this extensive dataset with over 2,500 cases assessed according to the molecular classifier with accompanying clinical data.
We will apply modern machine learning tools and develop a computer algorithm that is able to predict the four prognostic subgroups (or mutational profile) of endometrial cancer based on histopathology images from the tumour by inferring information from the tumour tissue that is not discernible to the human eye. This algorithm has the potential to be used clinically as a biomarker for prognostic classification5.
As above, the approach we will take will offer the opportunity to identify new biomarkers that is not genomic-based driving discoveries for precision medicine.

