Cervical Cancer
Success Measurement
Strategic Initiative
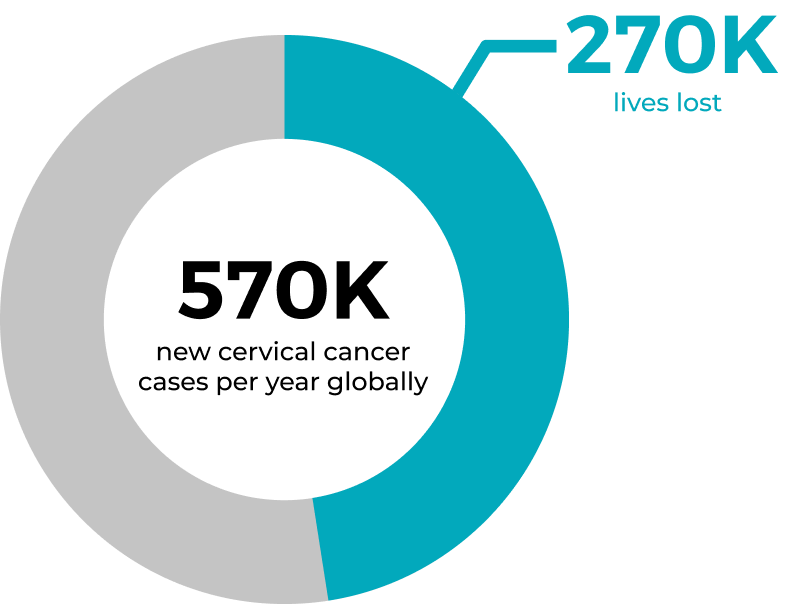
In Canada, 4-5 million pap tests are done per year in order to achieve a low rate of this invasive disease (1550 cases and 400 deaths) by catching the presence of abnormal cells early and treating them.
Canada is prepared to step up to the World Health Organization call to action to eliminate cervical cancer, and we believe that the Canadian opportunity is to demonstrate the capability of elimination. This is largely due to the discovery that a common Human papillomavirus (HPV) is linked to the development of cervical cancer.
HPV vaccination provides safe, effective and lasting protection against the HPV infections that most commonly cause cancer. However, despite great advances having been made in primary prevention with the HPV vaccine, secondary prevention and early treatment of pre-cancer remains vital to achieving the global goal.
Cervical cancer doesn’t have to be a death sentence, in fact cervical cancer doesn’t have to exist at all.
The Solution – “Pap” test
HPV is the most common sexually transmitted infection and three out of four women who are sexually active are at risk of contracting the virus. In most women, it clears on its own, while for others it becomes a persistent infection which leads to precancerous lesions. A vaccine can eliminate the acquisition of HPV altogether (which shows up in 99.7% of cervical cancer cases) or a Pap smear or an HPV screening test can catch these lesions before they become cervical cancer. BC Women’s Hospital + Health Centre, in conjunction with UBC Faculty of Medicine and BC Cancer are dedicated to the elimination of cervical cancer for women in British Columbia.
British Columbia’s Pioneering Track Record
In 1949, BC became the first jurisdiction in the world to introduce a publicly-funded cervical cancer screening program using the Papanikolaou smear or “Pap” test. This effort has led to a decline in deaths from cervical cancer in BC of over 70%.
BC is still leading the conversation on cervical cancer. BC Women’s Hospital and BC Cancer scientists have written national guidelines, informed international policies on prevention by increasing the vaccination uptake and creating innovative, cost effective screening to save women’s lives, including:
The tools are available to eliminate cervical cancer now, going forward this has to be translated into awareness and change of protocol and practice. Today, the GCI has an ambitious target to meet. It aims to eliminate cervical cancer in this province and across Canada, aligning directly with the World Health Organization’s call to action. With the unique datasets here in BC and the global expertise of the team, the GCI is uniquely positioned to undertake this ground-breaking initiative. The GCI’s cervical cancer specialists have identified key knowledge gaps which have informed the strategic priorities outlined below.
I. Vaccination
Impactful research, developed in British Columbia, has already informed practice and policy worldwide, reducing the HPV vaccination process from 3 to 2 doses; this sets the stage for their ongoing research in this area. Today, our BC scientists and clinicians are examining if 1 dose is as or more effective for Canadian girls. By following this group of Canadian girls prospectively, the team will determine if booster vaccinations are required. Currently, only 65% of girls eligible to receive the vaccine do so.
This initiative of the GCI will not only assess the impact of the team’s past discoveries on HPV vaccination on cervical cancer incidence and outcomes but will also strive to increase advocacy, education and awareness and innovate new tools to overcome any barriers that currently exist. Through education and better access, the goal is to improve the coverage of the vaccine to 90%.

II. Screening
The factors of access, financial resources, geographic obstacles, or culturally safe care inhibit women from going to be screened for cervical cancer. Creating innovative and cost-effective tools to reduce the access challenges is one of the key priorities identified by the GCI. The research team, working with colleagues across the country is looking to study how to implement the process of self-collection in BC and the rest of Canada. This will also help improve the availability of gynecological healthcare of rural, Indigenous and immigrant populations.
Cervical cancer screening currently lacks the ability to fully define a woman’s risk for the presence of the HPV progression to cervical cancer. By evaluating the bacterial and viral populations that live in the vagina we will be able to group women into high and low risk of developing cervical cancer. The research team is poised to use and advance our knowledge of the normal bacteria that naturally live in the vagina (the vaginal microbiome) to tailor diagnosis, treatment, and knowledge sharing in women’s reproductive health. As a result of the HPV FOCAL clinical trial, BC researchers have stored samples collected and individualized patient outcomes for ~6-10 years after diagnosis, which presents an unprecedented opportunity to determine associations between microbial populations, the cervicovaginal proteome and progression to cancer. This will reduce the number of inappropriate and stressful investigations and will set the stage for personalized screening and diagnostic approaches, moving us further towards the goal of elimination of cervical cancer.
In advancing these initiatives the GCI is inviting new expertise, approaches, and infrastructure to forge a leading-edge, cross disciplinary team. The overall goal is to use precision medicine approaches to tailor screening diagnostics, treatment, and knowledge translation for women’s gynecologic health. Positive outcomes are expected by creating and fostering expertise, synergies, data-sharing, and knowledge translation not only in BC but worldwide.
